In this first edition of Casebook for the year we focus on the impact a taxi tax could have on accessing healthcare in rural areas, a debate on rural dentistry, NHS targets, and how rural areas are missing out on specialised healthcare. Nigel Edwards, the National Centre for Rural Health and Care Chair, also provides a useful update on Centre activity. And there is a free seminar opportunity from one of our members too. Read on to find out more…
National Centre Update
There are many challenges in health and local government in rural areas and there is huge value in networks as a way to help people share ideas about how they are dealing with these. In my first few months as chair, I have been thinking about whether there is a need for more focused work to provide support to people who find themselves responsible for developing integrated health and care strategies for rural communities. The NHS is calling this place based leadership but it generally relates to District Council or small unitary authority areas and the approach should be a partnership not NHS dominated.
There is a lot being asked ranging from dealing with workforce shortages, reducing inequalities, improving prevention, developing more integrated ways of working and exploiting opportunities for economic development. Rural areas have particular problems but also assets and opportunities that can be built on. Many of the ideas and policies are developed by people with urban areas as their model and so there is a need for rural areas to work on their own version but also to use the capabilities and assets that are available.
I have identified a lot of people working on these issues who have expertise to share and I want to use the resources of the Centre and its partners to connect them with local leaders.
I am developing ideas for learning communities for people to share insights into the problems and solutions they are developing and learn from each other. This would include jointly working on approaches to creating change, providing a forum for bringing in external experts and policy makers and hopefully, to also make connections to others who they can learn from.
If you might be interested in this do drop me a line.
“Taxi Tax” threatens rural healthcare access
In a move that could disproportionately affect rural communities across the UK, the proposed 20% VAT hike on private hire and minicab journeys – colloquially termed the 'Taxi Tax' – is raising alarms about the accessibility of essential services, particularly healthcare.
A petition initiated by 38 Degrees, a platform advocating for social change, calls on the government to reconsider this increase. The concern is amplified in rural areas where public transport options are limited, and private hire vehicles are often the only means of transport for many, especially for attending medical appointments.
Recent discussions in the House of Commons have shed light on the struggles faced by rural residents. The proposed tax hike could significantly increase travel costs, making it increasingly challenging for those without personal transport, particularly the elderly and those with mobility issues, to access vital health services.
For instance, in areas like Selby and Ainsty, already limited to a handful of dental practices providing NHS services, the additional financial burden of the 'Taxi Tax' could make necessary healthcare visits unfeasible for many. The scenario is not different in other rural constituencies, where the nearest medical facility or essential service can be several miles away, necessitating reliance on private hire vehicles.
A report by the Express highlights the widespread opposition to this tax increase, citing concerns from various sectors, including business groups and women's safety charities. There is a fear that the tax could not only impact individual livelihoods but also the broader rural economy, where the availability of transport plays a crucial role.
As the debate continues, it's imperative to consider the unique challenges faced by rural communities. This situation calls for a nuanced approach that balances fiscal needs with the realities of rural life. The Rural Services Network urges the government to recognise the critical role of affordable transportation in rural healthcare access and to find solutions that support, rather than hinder, the health and welfare of rural residents.
Debate on NHS dentistry raises rural concerns
A debate in the House of Commons on 9th January raised concerns over the lack of NHS dentists available.
It cited a Nuffield Trust report into the State of NHS Dentistry which states that NHS funded dental services in England, ‘are in near terminal decline with nearly 6 million fewer courses of NHS dental treatment being provided last year than in the pre-pandemic year’.
Many MPs raised concerns faced by their constituents about the lack of access to NHS dentistry in their area, with Ashley Dalton MP stating that ‘in 2024 it is easier to get your hands on a Taylor Swift tickets than to get an NHS dental appointment!”
Selaine Saxby MP in North Devon shared her concerns in the debate:
“One of my concerns about the statistics used is that they compare dentists per 100,000 of population. As a very sparsely populated rural location, we might not look like as much of a dental desert as some other places, but at present the nearest dentist taking NHS patients is over 100 miles away.”
Sarah Dyke MP added:
“The shortage of dentists is a major issue that limits access to oral healthcare, especially for elderly residents who are at higher risk of dental decay and social isolation. There are specific challenges to rural dentistry provision, recruitment and retention. These need to be recognised because gaps in provision lead to gaps in teeth… I specifically want to see policies that address the lack of dentists in rural areas. Our communities are spread across a large geographical area, and if the one remaining dental surgery in a town such as Somerton or Castle Cary in my constituency cannot take on new patients, residents are faced with major obstacles to accessing a dentist. I want to see mobile dentistry hubs established to cater for rural communities that do not have dental provision.”
Ashley Dalton MP highlighted the difficulties the lack of transport options poses for finding alternative providers:
“When services are not available in Burscough, in my constituency, it is not as simple as phoning the next practice down the road, or the one just over from that. It means travelling to Skelmersdale, to Southport, to Liverpool. One of my constituents has contacted every practice in our constituency and beyond, from Ormskirk to Blackpool, and is unable to register anywhere as an NHS patient—and Blackpool is 50 miles away, a four-hour round trip by public transport.”
Transport concerns were echoed by Keir Mather MP from Selby and Ainsty:
“In Selby and Ainsty, we have been left with just nine dental practices offering NHS services; we have just nine for a vast rural constituency that stretches from Doncaster in the south to Harrogate in the north, and suffers fundamentally with issues such as a lack of public transport in our rural areas—it is simply not good enough.”
You can read more about the debate at this link
The Rural Services Network is concerned about the lack of NHS Dentist providers in rural communities.
Kerry Booth, Chief Executive of the RSN said:
“A core NHS principle is to provide services to all. Yet rural voters are disadvantaged due to poor access to transport, greater distance to receive timely care, a higher density of older people, the availability of affordable and appropriate housing stock and difficulties recruiting a healthcare workforce - all impacting on the health and care of rural voters. Rural voters deserve healthcare that is truly accessible and effective to all.”
NHS targets missed
The BBC reported this month on the key NHS targets that have never been met.
Research by the BBC shows that 'The analysis focused on the three key hospital targets, covering A&E, cancer and waiting times for planned care'.
Combined, the length of time during which the targets have been missed tops 100 years.
King's Fund think tank chief analyst Siva Anandaciva said the findings of the BBC analysis should "act as a wake-up call". "These are the key totemic targets," he said. "The length of time they have been missed is incredible."
Patients groups warned the delays were putting patients at risk.
Patients Association chief executive Rachel Power said the analysis showed the NHS was in "permacrisis". "The health of many deteriorates while they await treatment and their problems become more complex," she said.
A spokeswoman for NHS England said progress was being made, with the numbers facing really long waits falling and signs the NHS was coping better this winter than last.
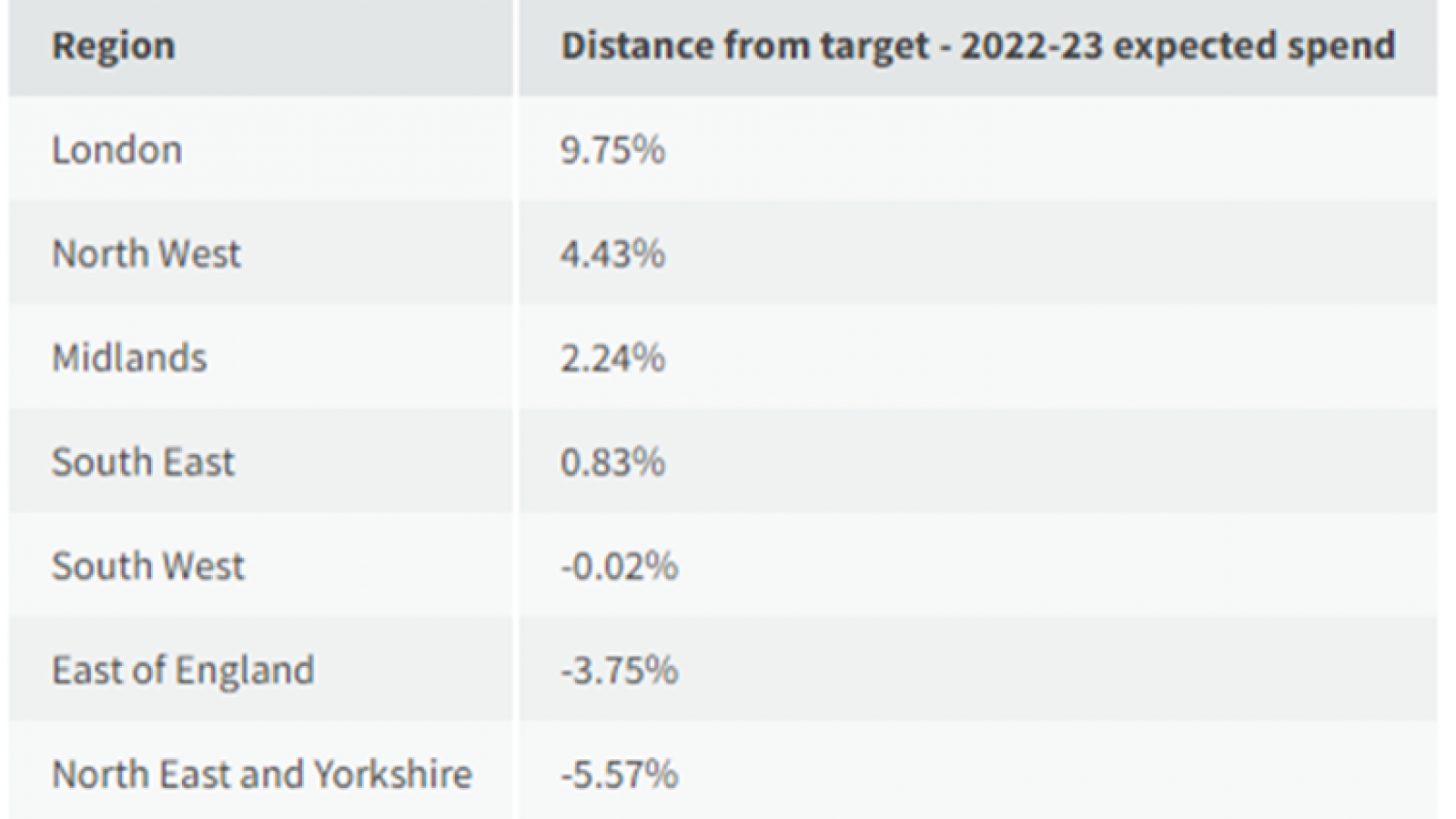
London gets well over fair share of specialised NHS services while rural areas miss out
The Health Service Journal recently reported on NHS England figures. HSJ findings suggest “people in some more rural areas are missing out on specialist treatments they should be getting, while Londoners are receiving a lot more than their fair share”.
The HSJ goes on to report that:
“First ICS (Integrated Care Systems) specialised service allocations reveal:
- Systematic shortfalls in access to remote communities.
- Spending on Londoners is 9.8 per cent over target.
- Suggests those living further from specialist services are missing out, including on cancer and cardiac treatment.
NHS England has suggested the main cause is “systematic shortfalls in access [in] remote communities”, leaving “unmet need” for specialised services in these areas.
However other factors, including coding and reporting practices, year-to-year fluctuation, and weaknesses in the formula, are also likely to be confusing the picture, sources said.
The variation is being uncovered now because NHSE is preparing to fund many specialised services via allocations to integrated care boards. These allocations will be based on estimates of their populations’ healthcare needs, rather than NHSE negotiating payments directly with provider trusts – as it has since 2013.
The national body published figures last month showing for the first time how much the current spending for each integrated care system compares to what its new allocation formula predicts should be spent.
The highest above its “fair share” target is South East London, at 22.2 per cent over, while Bedfordshire, Luton and Milton Keynes; Dorset; Northamptonshire and Somerset are all more than 10 per cent below.
West Yorkshire is 11.3 per cent below its fair share, despite housing Leeds Teaching Hospitals, which is a large city specialised provider.
London is the highest region above target by some distance (9.8 per cent), while the North East and Yorkshire are furthest below, at 5.6 per cent below (see table below).